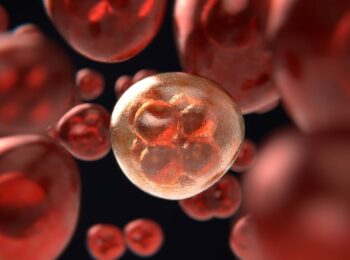
Inflammatory diseases and allergies increase with a decrease of human direct contact with nature. The modern lifestyle means that valuable bacteria required to keep the immune system busy is mitigated, a new study shows.
The study carried out at Karolinska Institute and University in Sweden and the University of Helsinki in Finland is based on a previous research project in Finnish Karelia where it was observed that children living in the countryside in close contact with nature are usually less allergic compared to children that live in cities.
The authors found that subjects living on farms or near forests had more diverse bacteria on their skin and lower allergen sensitivity than individuals living in areas with less environmental biodiversity, such as urban areas or near bodies of water.
Allergen-sensitive individuals had a lower diversity of one class bacteria, gammaproteobacteria, on their skin than healthy study subjects. The presence of one gammaproteobacterial member, Acinetobacter, was associated with the expression of the anti-inflammatory marker IL-10 in the blood of healthy study subjects. That suggested to the authors that gammaproteobacteria in the skin microbiota may enhance immune tolerance.
The study, published in the scientific journal Journal of Allergy and Clinical Immunology, confirms that the relationship between nature, bacteria, and health is not merely a coincidence – without a causal link.
In a second phase of the study, the researchers compared mice living in cages on the ground with mice that live in clean cages hanging off ground. The result shows that the intestinal flora of the mice that live on the ground changes in a beneficial way – they develop considerably more benign inflammation when subjected to artificial asthma.
The fact that the intestinal bacteria are important to our health is nothing new, they keep the immune system busy reduces the risk of immune system hypersensitivity to typically harmless substances in the environment.
Earlier research has also suggested that the dramatic increase in chronic inflammatory diseases in recent decades may be due in part to reduced contact with natural microorganisms, called the “hygiene hypothesis“.
The hygiene hypothesis suggests that a lack of early childhood exposure to infectious agents, symbiotic microorganisms (such as the gut flora or probiotics), and parasites increases susceptibility to allergic diseases by suppressing the natural development of the immune system. It is supported by epidemiological data, studies have shown that various immunological and autoimmune diseases are much less common in the developing world than the industrialized world and that immigrants to the industrialized world from the developing world increasingly develop immunological disorders in relation to the length of time since arrival in the industrialized world.
The researchers note that with a modern lifestyle, human beings can have lost a large part of the health-promoting bacteria that we lived together with for centuries of a common evolution. Now, when we do not have these bacteria around us to the same extent and therefore lost a vital latent stimulating factor for the immune system.
Reference:
Ilkka Hanski, Leena von Hertzen, Nanna Fyhrquist, Kaisa Koskinen, Kaisa Torppa, Tiina Laatikainen, Piia Karisola, Petri Auvinen, Lars Paulin, Mika J. Mäkelä, Erkki Vartiainen, Timo U. Kosunen, Harr. “Environmental biodiversity, human microbiota, and allergy are interrelated”. Proceedings of the National Academy of Sciences, May 7, 2012 DOI: 10.1073/pnas.1205624109