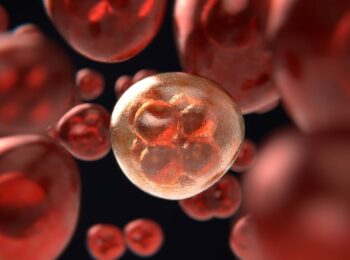
Two international research teams have now shown that tailor-made vaccines can be used aginst skin cancer, malignant melanoma. However, the vaccine is only given when cancer has been formed.
The vaccine cannot be taken in advance to protect against the disease. Instead, the reason for it to be called a vaccine is how it involves the body’s own immune system – activating the immune system to begin fighting tumor cells.
The research teams mapped the genes of a number of individuals’ respective tumors and also investigated how blood cells defended themselves against cancer. Then, the vaccine was created to activate the immune system even more so that it can attack the tumors.
The vaccines were created by harnessing cancer molecules personalized to each tumor, and by including them in the vaccines, it was possible to activate the body’s immune system, enable it to recognize the tumors and attack them. Afterward, it also kept any disease left behind at bay.
Various methods have been used to introduce the vaccine, either through subcutaneous injection or via ultrasound of the lymph nodes. It has been tested on six people in the United States and 13 in Germany.
In addition to malignant melanoma, patients with other cancers that mutate, thus change rapidly, would benefit from a similar treatment. This could include, for example, kidney cancer and cancer of the bladder.
The first study used the molecule RNA and the second used protein molecules. Both studies have been published in journal Nature under the names “Personalized RNA mutanome vaccines mobilize poly-specific therapeutic immunity against cancer”:
The cumulative rate of metastatic events was highly significantly reduced after the start of vaccination, resulting in a sustained progression-free survival.
Our study demonstrates that individual mutations can be exploited, thereby opening a path to personalized immunotherapy for patients with cancer.
and “An immunogenic personal neoantigen vaccine for patients with melanoma”:
Of six vaccinated patients, four had no recurrence at 25 months after vaccination, while two with recurrent disease were subsequently treated with anti-PD-1 (anti-programmed cell death-1) therapy and experienced complete tumour regression, with expansion of the repertoire of neoantigen-specific T cells. These data provide a strong rationale for further development of this approach, alone and in combination with checkpoint blockade or other immunotherapies.
However, the researchers note that more research is needed to check if these vaccines are better than the existing treatments, if they are able to improve survival rates and what their long-term effects would be.
Reference:
Patrick A. Ott et al “An immunogenic personal neoantigen vaccine for patients with melanoma” 5 July Nature 2017 doi: 10.1038 / nature22991
Ugur Sahin et al., “Personalized RNA Mutanome Vaccines Mobilize Poly-Specific Therapeutic Immunity Against Cancer” 5 July 2017, Doi: 10.1038 / Nature23003