Our inner clock can explain why long-term stress or corticosteroid medicine containing cortisone can lead to weight gain.
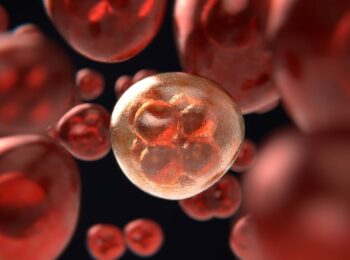
American researchers have studied how the body transforms specific precursor cells to fat cells, and how it is in turn affected by the stress hormone cortisol.
The levels of cortisol usually vary during the day, with higher levels in the morning to activate us after a nights sleep. However, our inner body’s clock can be disrupted when the body is receiving cortisol continuously or at times during the day. With our overactive endocrine glands of the brain result in the periodic release of hormones.
This can happen due to prolonged stress or in corticosteroid therapy with cortisone being converted into cortisol in the body. Medicinal products with cortisone are used, for example, in rheumatic diseases and severe asthma.
A healthy person’s level of glucocorticoids rises and falls in a circadian 24-hour cycle, peaking around 8 a.m., dropping to its lowest around 3 a.m. the next day, and then rising back to its peak about five hours later. The rise is a wake-up signal that gets us moving and turns on our appetites. The glucocorticoid levels in our bloodstream are also increased by stress — short spikes are induced by short-term stress, such as exercise, and sustained levels are caused by chronic stress.
The American researchers have now found that certain molecular processes in mice can be initiated when cortisol levels are high for a long time. These processes cause more cells to be converted into fat cells. When the cortisol levels remain high for more than 12 hours, the body starts to convert more fat cells.
Even though all the mice ate the same amount, only those implanted with glucocorticoids gained weight. The doubling of their fat mass was due to both the creation of new fat cells and the growth of existing fat cells.
“It explains why treatments with glucocorticoid drugs, which are often essential for people with rheumatoid arthritis and asthma to even function, are so linked with obesity, and it suggests ways in which such treatments can be given safely without the common side effects of weight gain and bone loss,”
– Mary Teruel, Ph.D., assistant professor of chemical and systems biology and senior author of the study.
The study results could be helpful in healthcare to reduce the risk of side effects in patients. The research results suggest that even if you get significantly stressed or treat your rheumatoid arthritis with glucocorticoids, you won’t gain weight, as long as stress or glucocorticoid treatment happens only during the day. But if you experience chronic, continuous stress or take glucocorticoids at night, the resulting loss of normal circadian glucocorticoid oscillations will result in significant weight gain
Reference:
Zahra Bahrami-Nejad et al. A Transcriptional Circuit Filters Oscillating Circadian Hormonal Inputs to Regulate Fat Cell Differentiation. Cell Metabolism April 3, 2018.